6 Signs of Heart Attack A Month Before: Heart Attack Warning
Prodromal symptoms, which occur in the month leading up to a heart attack, are comparable to those that occur during a heart attack. These include symptoms like palpitations, shortness of breath, and chest pain.
Each person’s experience is unique, and there are other symptoms that are less common. Some folks have absolutely no symptoms.
This article goes over the 6 Signs of Heart Attack A Month Before, as well as others that occur less frequently. It also discusses what happens just before a heart attack occurs.
Can Healthy People Have Heart Attacks?
Although many people believe that heart attacks and heart disease only affect older persons, this isn’t always the case. Young adults may acquire clogged arteries and other heart attack risk factors, such as high blood pressure and cholesterol.
Therefore, if you are worried about healthy people having heart attacks. Yes, it would be. Adults of all ages must therefore be aware of the warning signals of a heart attack.
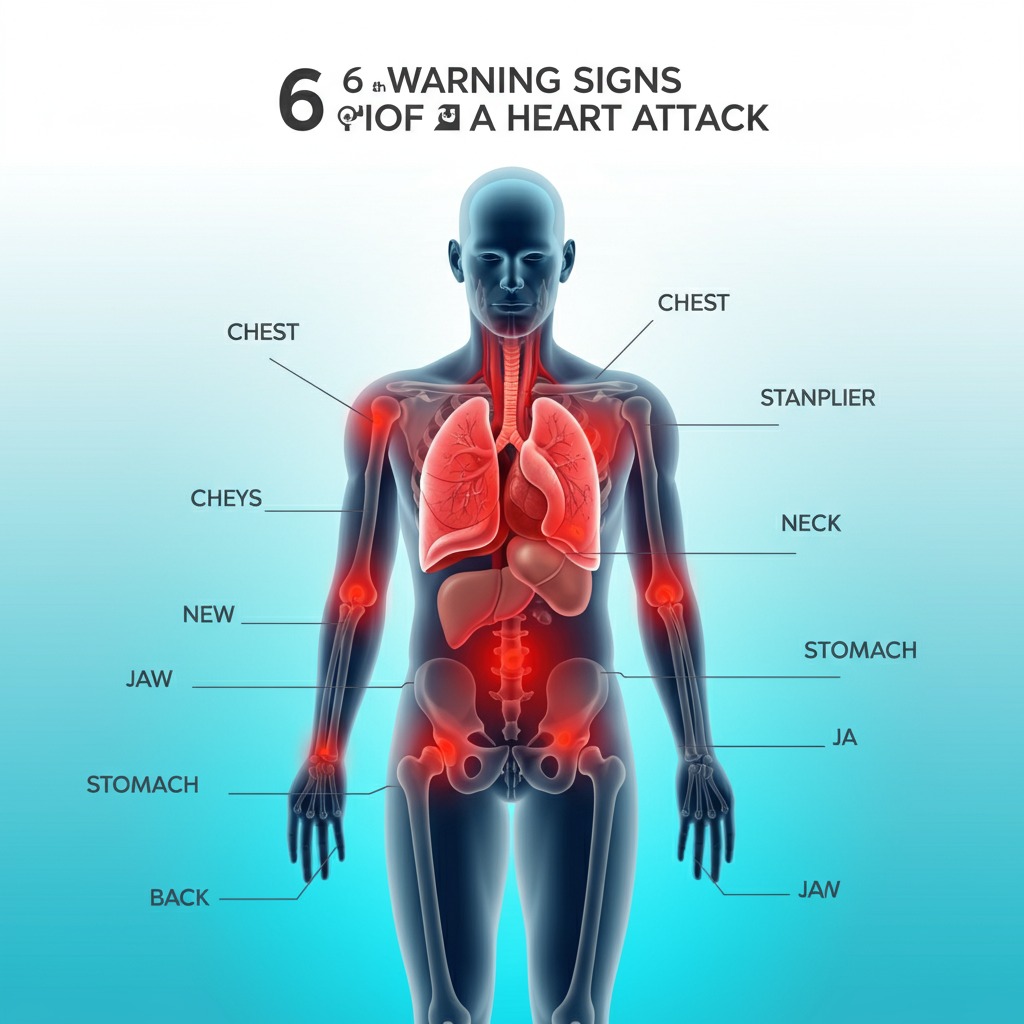
6 Signs of Heart Attack A Month Before
Identifying all 6 warning signals of a heart attack a month in advance can provide a key window for treatment. What you should know is this:
Chest Discomfort
The most well-known indication, although its length and intensity might vary significantly. While some people may feel minor discomfort or a burning sensation akin to indigestion, others may sense a heavy, pressing sensation. A lack of blood flow to the heart is one of the warning indications of a heart attack, and this could be one of them.
Shortness of Breath
Reduced cardiac function may be the source of your tendency to feel winded easily during activities that used to not elicit this reaction. This symptom is frequently disregarded, particularly by women, who may blame it on aging or a lack of fitness. It’s crucial to remember that shortness of breath is a common symptom of female anxiety and small heart attacks.
Fatigue
Unusual fatigue without a known cause may be a sign of an impending heart attack. Even basic chores like changing the bed or going to the restroom can become tiresome due to this extreme weariness.
Pain in Other Areas
Although it is a common symptom, pain can also be felt in other areas of the body, including the chest. This includes pain in the neck, jaw, stomach, limbs, or back. “How long do you have jaw pain before a heart attack?” is a question that many individuals ask. Any inexplicable pain in these places should be regarded seriously; however, the answer varies.
Digestive Issues
Before a heart attack, other symptoms may include heartburn, nausea, indigestion, or stomach discomfort. Although these symptoms are frequently confused with those of other, less serious disorders, they should be treated by a doctor if they continue or are accompanied by other symptoms on this list.
Sleep Disturbances
Heart issues may be the cause of trouble sleeping, remaining asleep, or waking up feeling exhausted. Heart disease patients frequently have sleep difficulties, which may be an early warning indication of an imminent heart attack.
Even though these symptoms can be intermittent and confused with other illnesses, they should not be disregarded, particularly if they are new or getting worse.

Risk Factors and Prevention
Understanding your risk factors is just as important as being aware of the warning signs of a heart attack. A family history of heart disease, smoking, high blood pressure, high cholesterol, obesity, diabetes, and a sedentary lifestyle are examples of common risk factors.
Lifestyle Modifications to Reduce Risk
- Frequent Exercise: Heart health can be enhanced by participating in at least 150 minutes of moderate aerobic activity or 75 minutes of strenuous activity per week.
- Healthy Diet: Heart disease risk can be decreased by eating a balanced diet high in fruits, vegetables, whole grains, and lean meats and low in sugar, salt, and saturated fats.
- Give Up Smoking: One of the main risk factors for heart disease is smoking. Your risk can be considerably decreased by giving up smoking.
- Control Stress: Prolonged stress raises the risk of heart disease. Stress management methods include deep breathing, yoga, and meditation.
- Frequent Checkups: Early detection of heart disease symptoms might be aided by routine health examinations. In order to detect cardiac issues before they worsen, Atrius Cardiac Care provides thorough diagnostic procedures.
Why Early Detection Matters?
Early identification of a heart attack is critical since it can prevent additional damage to the heart and potentially save lives. The cardiac muscle sustains more damage the longer the blood supply to the heart is cut off.
The absence of oxygen and blood flow during a heart attack can cause the heart muscle cells to die, causing irreversible damage. Restoring blood flow and reducing the severity of cardiac injury can be achieved with prompt intervention, such as medication or surgery.
Early identification also makes it possible to lower the risk of further cardiac events by implementing heart attack prevention techniques, including medication and lifestyle modifications. People can take preventative measures to safeguard their heart health by being aware of the warning signals and getting help right away.
How Many People Survive a Heart Attack?
A heart attack, also known as a myocardial infarction, occurs when blood flow to the heart is blocked, often due to a buildup of plaque in the coronary arteries. Immediate medical attention is crucial, and thanks to advances in emergency care and treatment, survival rates have improved significantly over the years.
Today, about 90% of people survive their first heart attack, especially if they receive prompt treatment. The chances of survival depend on various factors, including how quickly medical help is received, the severity of the heart attack, the person’s age, overall health, and whether they have other conditions such as diabetes or high blood pressure.
Many survivors can go on to live long, healthy lives with the help of medications, lifestyle changes, and cardiac rehabilitation programs. Quitting smoking, eating a heart-healthy diet, exercising regularly, and managing stress are vital steps toward recovery and preventing another heart attack.
However, while survival is common, a heart attack remains a serious medical event that can have lasting effects on the heart. Some individuals may experience heart damage or complications that require ongoing treatment.
Early recognition of symptoms—such as chest pain, shortness of breath, or discomfort in the upper body—is key to improving outcomes. Calling emergency services immediately at the first sign can save lives.
In summary, the majority of people do survive a heart attack with proper and timely care, and many make a strong recovery by committing to heart-healthy habits and following their healthcare provider’s advice.
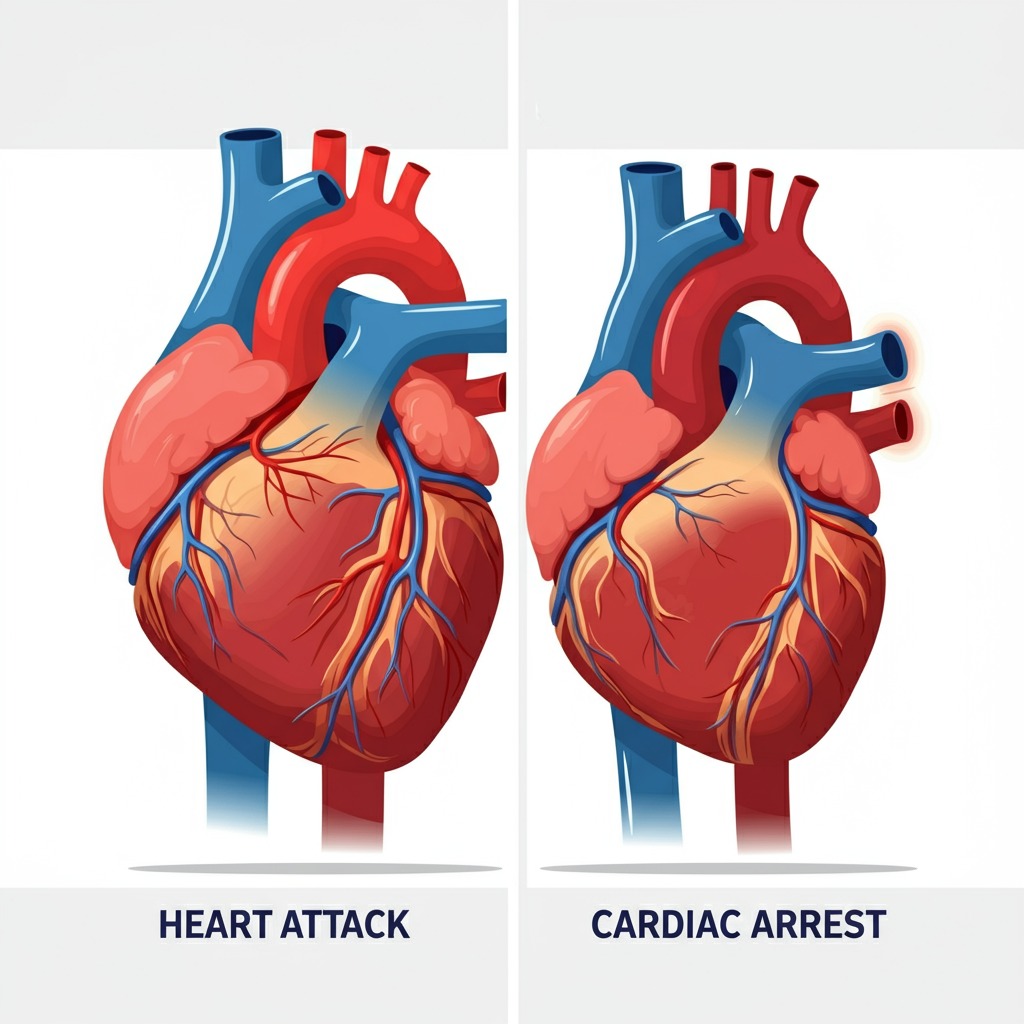
Difference Between Cardiac Arrest and Heart Attack
A heart attack and a cardiac arrest are both serious heart conditions, but they are very different in cause, symptoms, and treatment.
Heart Attack Happens
A heart attack happens when blood flow to part of the heart is blocked, usually by a blood clot or narrowed artery. This prevents oxygen from reaching the heart muscle, which can cause permanent damage if not treated quickly. Symptoms may include chest pain, shortness of breath, sweating, and nausea. The heart usually keeps beating, and the person is often conscious and responsive.
Cardiac Arrest Happens
In contrast, a cardiac arrest is a sudden, unexpected loss of heart function. It’s usually caused by an electrical malfunction that disrupts the heart’s rhythm (arrhythmia), causing it to stop pumping blood effectively. The person collapses, becomes unresponsive, and stops breathing. Without immediate CPR and defibrillation, cardiac arrest can lead to death within minutes.
While a heart attack can sometimes lead to cardiac arrest, the two are not the same. A heart attack is a circulation problem, while cardiac arrest is an electrical problem.
Understanding the difference is crucial: a heart attack needs urgent medical care, but a cardiac arrest is a life-threatening emergency that requires immediate CPR and defibrillation.
Final Words
For prompt intervention, it is essential to identify the modest heart attack symptoms one month in advance. Early signs, such as increased perspiration or unusual weariness, should not be disregarded. It is essential to comprehend the differences in symptoms between men and women as well as the importance of early detection.
Heart attack prevention is greatly aided by lifestyle choices such as frequent health screenings, stress management, diet, and exercise. By taking proactive steps to prioritize heart health, the risk of cardiovascular events can be considerably decreased. Keep yourself updated, pay attention to your body, and get help if you have any alarming symptoms. Your heart is worthy of care and attention.
Frequently Asked Questions